|
Author: Professor Zhao Ni, Department of Electronic Engineering
The global elderly population is growing at an unprecedented rate, particularly in low- and middle-income countries. According to World Population Prospects, by 2050, one in six people in the world will be over the age of 65 (16%), up from one in 11 in 2019 (9%). This demographic shift presents significant healthcare challenges, most notably the rising prevalence of cardiovascular diseases (CVDs). CVDs, including conditions such as coronary heart disease, stroke, and heart failure, are the leading cause of death and disability among older adults, accounting for 32% of all global deaths in 2019.
Early detection and continuous monitoring of cardiovascular risk factors are crucial for preventing and managing CVDs. High blood pressure is a major risk factor for CVDs and related mortality. Experts, including the American Heart Association, recommend regular blood pressure monitoring as a key strategy in managing this risk. Furthermore, research shows that long-term increases in average blood pressure, short-term variability, and nighttime blood pressure are closely linked to the development of cognitive impairment and dementia. Continuous monitoring of blood pressure and other vital signs is therefore essential in managing both cardiovascular and cognitive health. However, neither the traditional cuff-based blood pressure monitors nor consumer electronic gadgets can provide such type of functions.
Our project, supported by the RAISe+ Scheme, focuses on developing innovative wearable sensors for continuous cardiovascular monitoring. Building on our experience in wearable technology and physiological modeling, we created the first low-power sensors for continuous blood pressure tracking. We discovered that organic semiconductors, typically seen as low-performing plastics, can be engineered to outperform traditional silicon-based electronics in photodetection. In recent years, we've combined sensor innovation with advanced manufacturing and cardiovascular modeling to improve functionality and scalability. Our patented multi-wavelength photoplethysmogram model set a record for cuffless blood pressure (BP) measurements, offering the lowest measurement error while tracking heart rate, BP, respiratory rate, and blood oxygen with a single optical module. By introducing deep-learning approaches we further demonstrated high measurement accuracy over extended periods. Beyond BP tracking, we've developed models to detect cardiovascular parameters previously inaccessible to wearables, like stroke volume allocation (SVA) and systemic reflection coefficient (SRC). The combined sensor models achieve 91.18% accuracy in predicting heart damage and 88.51% accuracy in detecting mild to moderate cognitive impairment.
Through the RAISe+ project we will develop commercial products capable of continuously tracking of blood pressure alongside other vital signs, including heart rate, blood oxygen levels, arterial stiffness, and more. This comprehensive monitoring system is made possible through the integration of various medical-grade wearable devices, such as continuous blood pressure monitors, 12-lead electrocardiography (ECG), impedance cardiography (ICG), and phonocardiography (PCG). All of this data feeds into the second component of our project: a Personalized AI-powered virtual doctor, known as Dr. PAI. Utilizing Large Language Model (LLM) technology, like Chat-GPT, Dr. PAI is designed to understand patient inquiries and provide relevant responses and recommendations. The combination of real-time wearable data acquisition with advanced AI technology opens new horizons in personalized healthcare. This system not only offers continuous health insights for patients, especially the elderly with CVDs, but also provides healthcare providers with comprehensive data to monitor disease progression more effectively.
Although it might seem like Dr. PAI could replace a clinic visit, the project’s goal is to offer immediate health insights rather than substitute for doctors. The intention is to help patients, especially those with CVDs, better understand their health status while providing doctors with comprehensive data for effective disease monitoring. Dr. PAI is designed to complement traditional healthcare, particularly in regions with limited access to medical services. In many parts of the world, including public hospitals in Hong Kong, securing a timely appointment can be challenging due to resource constraints. Dr. PAI aims to bridge these gaps by enhancing access to medical expertise and improving patient care.
In summary, this project seeks to translate years of research in biomedical sensing and health informatics into advanced wearable devices capable of continuously and accurately monitoring cardiovascular disease (CVD) risk factors. These devices will be integrated with a personalized AI-powered virtual doctor, Dr. PAI, which utilizes generative AI models for real-time CVD prediction and diagnosis within a unique human-and-sensor-in-the-loop framework. The platform will undergo extensive clinical trials in Hong Kong and mainland China, with optimization and standardization led by an interdisciplinary team of cardiologists and eldercare experts. This innovative approach aims to revolutionize personalized healthcare, particularly in eldercare and CVD management, paving the way for improved health outcomes and quality of life for the global aging population. 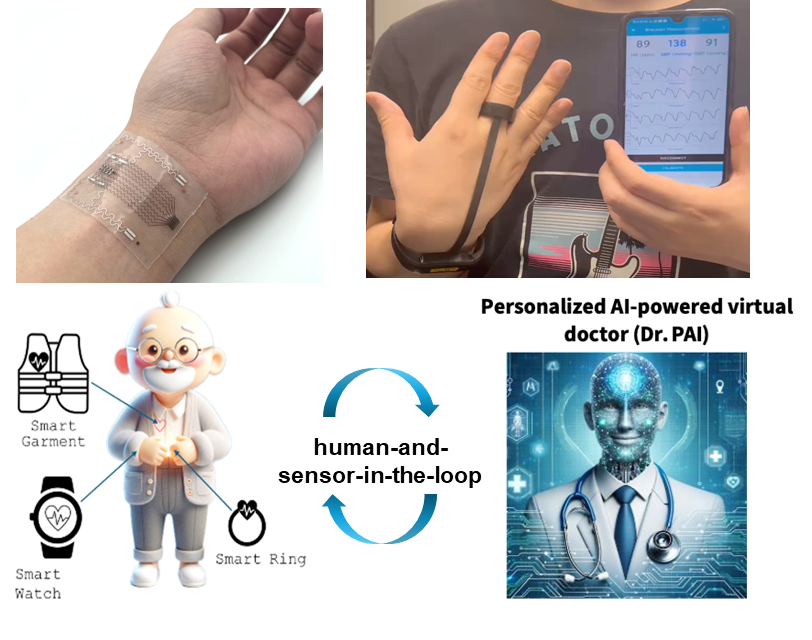  Professor Zhao Ni and her project members Professor Zhao Ni and her project members |
